The interviews reveal a medical workforce still struggling to adapt to dangerous conditions with little confidence that the available protective gear is being steered to the places it’s needed most. Some say they’re still being forced to reuse masks or MacGyver their own equipment four months into the U.S. outbreak, even as Trump dismisses questions about shortages as “fake news,“ as he did earlier this month.
“We had very little in our stockpile,” Trump said in a recent briefing. “Now we’re loaded up. And we also loaded up these hospitals.”
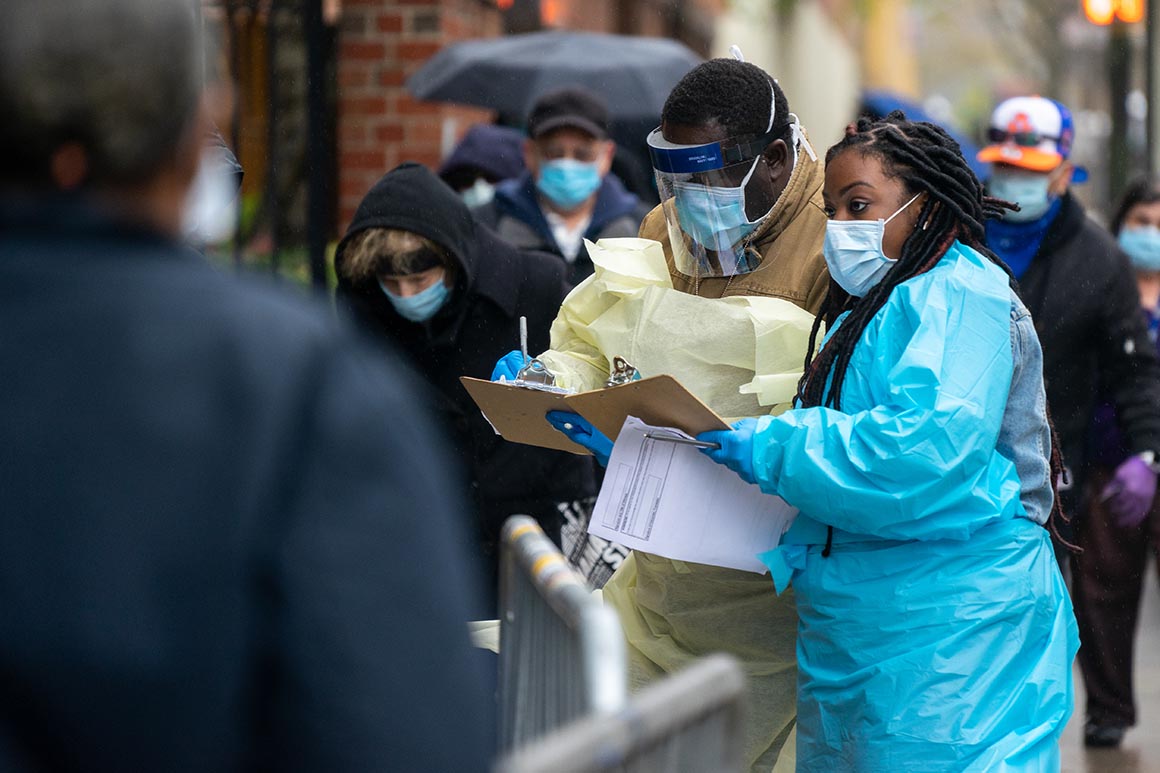
Without a more robust supply of personal protective equipment, or PPE, the fast-moving virus will continue to pose an unprecedented threat to America’s health care workforce, having already sickened at least 9,282 medical workers and killed 27. Those grim numbers, which come from a CDC report almost two weeks ago, are certainly an undercount.
And enduring shortages of protective gear could also set back timelines for reopening parts of the country and make it more difficult for cash-starved hospitals to resume elective procedures. Trump’s own guidelines say states should have adequate supplies of protective and medical equipment before dialing back social distancing restrictions.
States and hospitals say they have faced unusual challenges in their scramble to secure PPE — from a strained global supply chain and the Trump administration itself. They complain Trump’s encouragement of states to hunt down supplies on their own has created a chaotic competition for PPE and medical equipment. In some cases, states have accused the federal government of seizing shipments of protective equipment to distribute to another region, though the Federal Emergency Management Agency has denied those claims.
In interviews, doctors and nurses described restrictive hospital policies limiting workers to a single mask per day, though the equipment is supposed to be discarded after a single use to lower the risk of spreading infection. Others said workplace guidelines aimed at conserving gear are constantly shifting with little explanation of why. They described hospital administrators keeping unusually close tabs on their supply, and workers report being reprimanded for using basic protective gear outside of units designated for coronavirus patients.
“There’s no way that anyone could possibly think that what is happening now is acceptable, even in its improved form. It’s still not enough,” said a hospital physician in Georgia who requested anonymity. “To feel that you can’t do your job without begging, especially if you’re putting your body on the line, that you can’t get the tools you need without being gaslighted or interrogated, there’s something belittling and patronizing about it.”
Because of supply shortages, she said nurses at the safety-net Atlanta hospital where she works have wrapped stethoscopes in medical gloves to reuse them on multiple coronavirus patients, instead of following the recommended practice of using a dedicated disposable stethoscope for each patient. While mask supplies have improved, some doctors who worry about future shortages are keeping backup stashes in brown paper bags, she said.
Surveys of health care workers across the country appear to echo their concerns. A majority of those treating Covid-19 patients said they were worried about shortages of a vast array of protective equipment, including isolation gowns, N-95 masks and face shields, according to a poll earlier this month from the health services firm Premier. Additionally, 70 percent said providers were reusing masks to save supplies.
There are some small signs of improvement, however. While most critical care physicians in California said they were worried about protective equipment shortages, the most extreme concerns have faded since early April, according to a survey by the California Health Care Foundation.
A spokesperson for FEMA, which is overseeing the federal government’s distribution of supplies, said the agency has received „a number of requests for assistance from states and localities to fill PPE shortages.“ The Trump administration, as it works across the government and with industry to locate more PPE, has already sent out 66.9 million N-95 respirator masks, 105 million surgical masks and roughly 14 million gowns, the spokesperson said.
Still, states and health workers say they need more to fight a stealthy and highly contagious disease that Trump’s health experts believe will still be here in the fall.
Groups representing long-term care facilities including nursing homes say they still haven’t been prioritized for PPE, even though the virus has ravaged their high-risk populations. Thousands of deaths in long-term care facilities have been linked to the coronavirus, and more than 650 facilities have reported cases.
The American Health Care Association, the national group for long-term care providers, said three-quarters of its members are running out of PPE, and about 60 percent are reusing or improvising PPE.
Source: politico.com
See more here: news365.stream






